Carotid Artery Disease & Stroke Prevention
 Each year more than 500,000 people become the new stroke victims in the U.S. It is the third leading cause of death in the U.S. and it is responsible for some of the biggest expenditures in health care dollars in America. Not to mention there is an enormous incalculable cost in lifestyle adjustment and rehabilitation to the individual and their family in a patient who has had a stroke.
Each year more than 500,000 people become the new stroke victims in the U.S. It is the third leading cause of death in the U.S. and it is responsible for some of the biggest expenditures in health care dollars in America. Not to mention there is an enormous incalculable cost in lifestyle adjustment and rehabilitation to the individual and their family in a patient who has had a stroke.
Stroke is a disease of the blood vessels that affects the brain. A stroke occurs when a blood vessel to the brain suddenly bursts or becomes blocked. This part of the brain then begins to die. Nerves from this part of the brain no longer have control over part of the body. The result is usually permanent because the body cannot replace brain cells. Such brain injury may affect the ability to speak, to move the arms, to move the legs or to move the facial muscles. A stroke may affect behavior patterns, thoughts, memory, emotions, or sensations. Paralysis or weakness of one side of the body is common.
What is Carotid Artery Disease?
Carotid artery stenosis is the narrowing of the carotid arteries. The carotid arteries are the main arteries in the neck that supply blood to the brain. When atherosclerotic plaques develop in the arteries, the carotid arteries are often involved, causing the narrowing. These plaques are formed from cholesterol, fat and other substances that arise from the lining of the arteries. These atherosclerotic plaques in the carotid arteries are a risk factor for stroke.
Once an aneurysm ruptures, 50% of those with the aneurysm die before they reach the hospital.
Symptoms of Carotid Artery Disease
Carotid artery stenosis may or may not cause symptoms. A doctor may hear an abnormal sound when listening to the artery with a stethoscope. Carotid ultrasonography may also detect the stenosis by placing an ultrasound probe on the neck.
Treatment Options for Carotid Artery Disease
 Treatment of carotid artery stenosis depends on the degree of narrowing in the blood vessel. The greater the degree of stenosis, the more likely that a stroke will occur. Treatment of the stenosis may result in a dramatic reduction in the chance of stroke. Treatment regimens include medications, plaque removal, and plaque dilatation.
Treatment of carotid artery stenosis depends on the degree of narrowing in the blood vessel. The greater the degree of stenosis, the more likely that a stroke will occur. Treatment of the stenosis may result in a dramatic reduction in the chance of stroke. Treatment regimens include medications, plaque removal, and plaque dilatation.
Medication for the treatment of carotid plaques includes classes of drugs known as antiplatlet agents and cholesterol lowering agents. Antiplatlet agents such as aspirin reduce clots in the blood vessels. Cholesterol lowering agents known as statins control levels of blood cholesterol and may decrease the inflammation of the plaques. Medical treatment of hypertension and diabetes also prevents strokes.
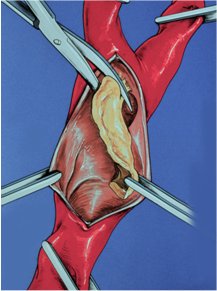
Medical therapy is the first line treatment of carotid stenosis and should be used for most blockages less than 50%. Narrowing of carotid arteries greater than 70% or plaques with dangerous ulcers should be considered for more aggressive therapies. These plaques are treated with procedures to remove the blockages. Treatment has the potential to reduce relative stroke risk by over 70%.The most commonly performed procedure is known as carotid endarterectomy. Carotid endarterectomy removes all of the plaque that caused the artery to narrow. These procedures have been shown to reduce the risk of stroke by between 50 and 70%. Another treatment is carotid artery stenting, which uses balloons and stents to dilate the plaques. This method is particularly useful for high-risk patients or plaques in unusual places.
FAQs
During your office visit, you will discuss the procedure with one of our physicians and he will select the most appropriate procedure for your treatment. Preprocedural testing requires blood tests, cardiac evaluation and special imaging studies of the arteries.
Most procedures require two or three days of admission to the hospital. You will be admitted to the hospital in the morning of the procedure. After the procedure is completed you will be admitted to the vascular unit of the hospital. Once you are discharged, you will return to our office usually about two weeks after the procedure. You will be seen in surveillance about every six months after the procedure for follow up ultrasonography to monitor for the small chance that the plaque will return.
The internal carotid arteries are large vessels which travel along both sides of the neck and provide blood flow to the brain.
Plaque can develop in these arteries. Plaque is basically made up of debris containing cholesterol, fatty acids, and calcium. This is the same type of plaque that can develop in the arteries of the heart and lead to heart attack. However, when it develops in the internal carotid arteries, it has the potential to lead to stroke. Strokes from the carotid arteries occur when a piece of the plaque breaks off, lodges in a small vessel, and restricts oxygen delivery to the brain.
When an individual is found through diagnostic testing to have plaque in the carotid arteries, a referral is often made to the vascular surgeon. The surgeon will review the imaging studies and determine to what degree the carotid artery is narrowed by the plaque. Based on this the surgeon is able to provide an estimate of the risk for stroke.
This determines the treatment plan. If it is felt that the risk for stroke is sufficiently low, conservative management with medications and modification of cardiac risk factors may be recommended. If it is thought the risk for stroke is high, procedural intervention will likely be considered.
There are several risks associated with carotid procedures. Some of these risks include:
- Stroke
- Bleeding
- Heart-related complications (including heart attacks)
- Localized nerve damage
- Re-narrowing of the artery
Doctors who recommend treatment have considered these risks and will only recommend a procedure if they feel the risks are acceptable, or if the risks associated with not having the procedure are significantly higher.


