- Are PAD and PVD the Same Disease?
- How is PAD Connected to PVD?
- What are the Symptoms of PAD and PVD?
- What Are the Treatment Options for PAD and PVD?
Have you ever wondered if peripheral vascular disease (PVD) and peripheral artery disease (PAD) are the same? In vascular health, these terms are frequently used interchangeably, which many may find confusing. PAD affects 8 to 12 million people in the United States alone. But are these statistics inclusive of all types of PVD, or is there more to the story?
There are more distinctions between PAD and PVD, though they are very similar. At Vascular Specialists of Central Florida, we want to keep you informed and educated on vascular health to prevent further confusion. Here are the symptoms, causes, and treatment options you should consider if you’re concerned about either disease.
Are PAD and PVD the Same Disease?
No, PAD and PVD are different. Peripheral Artery Disease (PAD) and Peripheral Vascular Disease (PVD) are often used interchangeably, however. Here is why:
Peripheral Artery Disease (PAD)
Peripheral Artery Disease (PAD) is a vascular condition that primarily affects the arteries and blood vessels that carry oxygen-rich blood from the heart to various body parts.
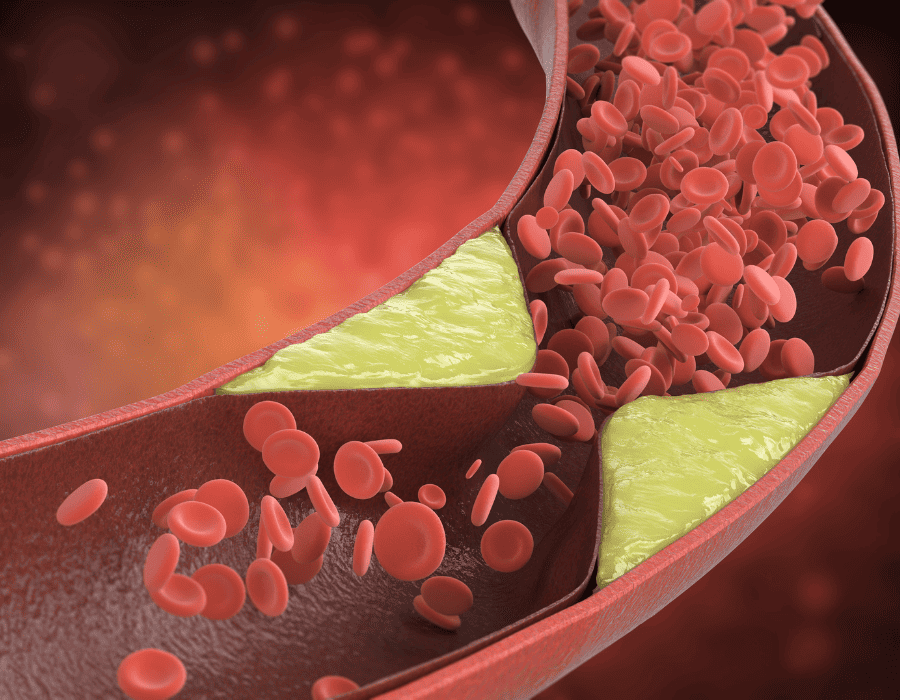
In PAD, these arteries become narrowed or blocked due to the buildup of plaque—consisting of cholesterol, fat, and other substances—on the inner walls of the arteries. This narrowing, also known as atherosclerosis, restricts blood flow to the limbs, most commonly affecting the legs.
Peripheral Vascular Disease (PVD)
Peripheral Vascular Disease (PVD) is a broad term for various vascular conditions that affect the blood vessels outside the heart. The vascular system includes arteries, veins, and lymphatic vessels that carry blood and fluid throughout the body.
PVD can manifest in different forms, and it may affect both arteries and veins. One common form is chronic venous insufficiency, which affects the veins and can lead to blood flowing backward, causing damage to tissues.
What Causes PAD and PVD?
 Peripheral Artery Disease (PAD) and Peripheral Vascular Disease (PVD) have diverse causes, reflecting the complexity of vascular health.
Peripheral Artery Disease (PAD) and Peripheral Vascular Disease (PVD) have diverse causes, reflecting the complexity of vascular health.
Causes of Peripheral Artery Disease (PAD)
- Atherosclerosis: The buildup of plaque in the arteries is the leading cause of PAD. Plaque, comprising cholesterol, fat, and other substances, narrows or blocks the arteries, limiting blood flow to the limbs.
- Blood Clots: Blood clots can also obstruct arterial flow, contributing to PAD.
- Injuries to Arteries: Trauma or injury to the arteries can lead to PAD.
- Irregular Anatomy: The unusual anatomy of muscles or ligaments may contribute to PAD.
- Infection: Infections affecting the arteries can be a rare cause.
Causes of Peripheral Vascular Disease (PVD)
- Atherosclerosis: Similar to PAD, atherosclerosis plays a significant role in PVD, affecting both arteries and veins.
- Injuries and Trauma: Injuries to blood vessels, whether arteries or veins, can contribute to PVD.
- Irregular Anatomy: Anomalies in the structure of muscles or ligaments may lead to PVD.
- Infection: Infections impacting the vascular system, including veins, can contribute to PVD.
- Genetic Factors: There may be a genetic predisposition to vascular diseases.
What Are the Symptoms of PAD and PVD?
These symptoms can vary in severity and may indicate different stages of the disease. Seeking medical attention for an accurate diagnosis and appropriate management is essential when experiencing any of these symptoms.
Peripheral Artery Disease (PAD) Symptoms
- Intermittent Claudication: Leg pain, cramping, or weakness during physical activity that typically resolves with rest.
- Numbness or Weakness: Reduced sensation or muscle strength in the affected limbs.
- Changes in Skin: Skin on the legs may appear shiny, thin, or have a bluish tint.
- Slow-Healing Wounds: Wounds or ulcers on the feet or legs may heal slowly or not at all.
- Cool or Cold Extremities: Legs or feet may feel cool to the touch compared to the unaffected limb.
- Poor Nail Growth: Toenails may grow thicker or more slowly than usual.
Peripheral Vascular Disease (PVD) Symptoms
- Swelling: Swelling in the legs, ankles, or feet.
- Skin Changes: Discoloration, reddish-blue tint, or thin, brittle, shiny skin on the legs and feet.
- Numbness and Tingling: Sensations of numbness or tingling in the legs.
- Varicose Veins: Twisted, enlarged veins visible under the skin.
- Pain: An aching or burning sensation in the legs.
- Restricted Mobility: Difficulty standing for extended periods.
- Itchy, Dry Skin: Skin on the legs may become dry and itchy.
- Erectile Dysfunction: In some cases, PVD may contribute to erectile dysfunction in men.
What Are the Treatment Options for PAD and PVD?
Effective treatment for PAD involves medications, lifestyle changes, and, in advanced cases, procedures like revascularization.
PVD treatments vary based on the specific condition but may include elevation, compression stockings, exercise, and medical interventions.
What are the Risk Factors for PAD and PVD?
 Genetics: Are Some More Likely to Develop It?
Genetics: Are Some More Likely to Develop It?
Certain individuals might have a higher chance of getting PAD or PVD because of their family history. These conditions might show up more often in specific families or ethnic groups because of certain inherited traits.
Lifestyle Choices: How They Affect Vascular Health
The choices we make daily can increase our chances of getting PAD or PVD. Not being active enough, having an unhealthy diet, and smoking are all linked to a higher risk of these diseases.
Age Impact
Getting older can make someone more likely to have PAD or PVD. As we age, our blood vessels naturally change. Over time, they may become less flexible and develop plaque deposits—made up of fats, cholesterol, and other substances—along their walls. This process, known as atherosclerosis, can narrow the arteries and impede blood flow to various body parts, particularly the legs.
Medical History and Other Health Conditions
Having a history of high blood pressure, diabetes, or heart problems can make someone more likely to get PAD or PVD. Understanding how these conditions connect helps in finding these diseases early and managing them better.
Can You Prevent PAD and PVD?
Prevention is the cornerstone of vascular health. Embrace a healthy lifestyle by exercising regularly, maintaining a balanced diet, and avoiding smoking. Controlling conditions like high blood pressure and diabetes is crucial. Early detection through regular check-ups ensures prompt intervention and can prevent the progression of milder forms.
Understanding the nuances between PAD and PVD is important for maintaining optimal vascular health. If you are experiencing any symptoms or have concerns about your vascular health, don’t hesitate to schedule an appointment with a vascular specialist at Vascular Specialists of Central Florida, Inc. Take a proactive step towards a healthier future.
