Deep Vein Thrombosis (DVT)
 When a blood clot occurs in a deep vein, predominantly in the leg, it is known as deep vein thrombosis (DVT).
When a blood clot occurs in a deep vein, predominantly in the leg, it is known as deep vein thrombosis (DVT).
DVT and it’s potentially fatal offshoot, pulmonary embolism (PE), collectively are known as venous thromboembolism (VTE). Together DVT and PE impact more than 600,000 Americans annually and produce more fatalities than breast cancer and AIDS combined.
“We can get DVTs in our body for many different reasons, but universally it presents with an all-of-a-sudden change in the amount of swelling in your leg, on one side or very uncommonly both sides,” says Adam B. Levitt, M.D., R.V.T., F.A.C.S., a board-certified vascular surgeon at Vascular Specialists of Central Florida.
What Causes DVT?
“DVT can happen after trauma, after prolonged immobility, or in patients that have a known or unknown cancer, among other reasons,” says Dr. Levitt.
It can also develop when individuals have illnesses that affect blood clotting, as a result of an accident, or when confined to a bed in a hospital or nursing home.
DVT should be treated as a serious condition. A blood clot in the veins can break free and move through the bloodstream to the lungs, impeding the blood vessels there, and causing low oxygen levels, lung damage, and even heart failure. When a DVT blood clot has reached the lungs it is known as a pulmonary embolism (PE).
People more than 60-years-old, people who smoke, who are overweight, and who have relatively sedentary lifestyles are at increased risk of developing DVT.
Eight million Americans suffer from PAD. Only 50% of PAD amputees survive more than four years.
Signs and Symptoms of DVT
 DVT can sometimes come about without any obvious symptoms, and even when symptoms do present themselves, it can appear like a wide range of other health conditions.
DVT can sometimes come about without any obvious symptoms, and even when symptoms do present themselves, it can appear like a wide range of other health conditions.
Some sudden signals that DVT may be present include:
- Swelling in one leg (and rarely in both legs)
- Pain, tenderness, or a feeling of cramping in the leg
- A warm feeling on the skin of the leg
- Reddish skin on the leg
- Visible veins on the leg
- Weak or tired legs
To diagnose DVT, a board-certified vascular surgeon will conduct a full physical exam of the legs, may order blood testing, and use imaging tests such as an ultrasound or a CT scan.
How is DVT Treated?
The goals of DVT treatment are to stop the blood clot from growing, to prevent it from breaking free and travelling to the lungs or to other organs, to inhibit long-term leg pain and complications, and to avert future blood clots from occurring.
“The classic treatment for DVT is anticoagulation, or thinning the blood, which can be done with several different medicines, most commonly Coumadin, but also Lovenox, and Xarelto,” says Dr. Levitt. “Depending on where your DVT is and your other associated health and comorbidities, sometimes we can treat that and actually dissolve the clot to help relieve the pain and pressure in your leg.”
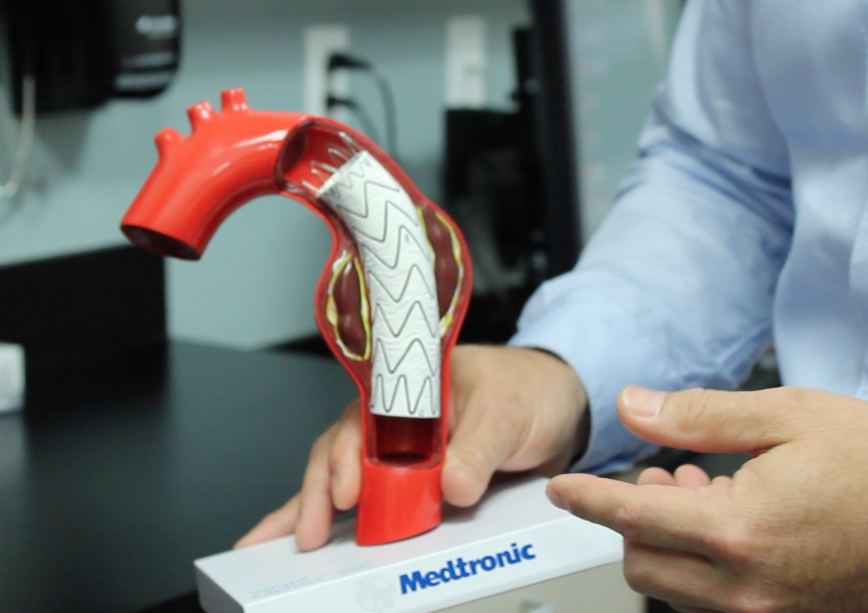
If a large blood clot is present or if a patient possesses a higher risk for PE, one’s physician may recommend catheter-directed thrombolysis, a minimally-invasive procedure where the surgeon uses the tip of a catheter to inject clot-busting medication directly into the clot.
“(Catheter-directed thrombolysis) is most commonly done when the DVT extends from the level of your groin up into your pelvis and less commonly if it involves the thigh,” says Dr. Levitt. “This is done in an interventional suite with contrast and usually involves one or two procedures, sometimes slightly longer. But the gold standard, the classic treatment is anticoagulation (medication).”
Compression stockings are commonly prescribed by doctors to help prevent swelling and the pooling of blood in the leg which can lead to clotting. Leg elevation can also help prevent long-term damage from DVT.
“I also recommend compression stockings as well as leg elevation long-term, for at least two years to prevent post thrombotic syndrome or a chronic debilitating problem with the legs from the DVT,” says Dr. Levitt. “Also while you’re sleeping, a pillow or two to elevate can help but sometimes this is unnecessary.”

